Abstract
Introduction
The classic chronic Philadelphia-negative chronic myeloproliferative neoplasms (MPN) are acquired stem cell diseases and include essential thrombocythemia, polycythemia vera, primary myelofibrosis and unclassifiable MPN. Recently, these disorders have been described as "A Human Inflammation Model for Cancer Development", reflecting chronic inflammation to be a major driving force for clonal evolution and disease progression in MPNs.
The objectives of this meta-analysis were to investigate if cigarette smoking is associated with increased blood cell counts (CBC) and incidence of MPN as proof of concept.
Method
A systematic review and meta-analysis was undertaken using databases Pubmed, EMBASE, Web of Science and World Health Organization Global Health Library for all relevant papers published until 15th February 2017 on smoking and complete blood counts and on smoking and myeloproliferative neoplasms according to a formal protocol that followed the PRISMA guidelines.
Following data extraction, STATA 13.0 was used to calculate raw and standardized mean differences for CBC (in SI units) and pooled odds ratios for MPN with 95% confidence intervals using random and fixed effects models. Main analyses included analyses of current smokers, ex-smokers, and ever smokers vs. non- or never smokers. Heterogeneity was measured using I2 -statistical analysis and Cochrane Q statistic, and reported corresponding p-values and sensitivity analyses included among others gender and smoke dosage(heavy (>=20 cigarettes/day) and light(<20 cigarettes/day)). Funnel plots, Egger's test and Begg's tests were used to assess publication bias.
Results
Complete Blood Count (CBC): A total of 88 references published from 1974-2017 in 10 different languages and including 90 study populations with 533,242 individuals, 222,887 current smokers, 92,001 ex-smokers, and 222,538 non-smokers between the ages of 15 and 89 from 34 countries were analyzed.
Meta-analyses showed that the mean of most CBCs were higher in smokers and ex-smokers compared to non-nonsmokers. Differences were larger comparing smokers to non-smokers than comparing ex-smokers to non-smokers, and also larger comparing heavy smokers to non-smokers than comparing light smokers to non-smokers. Furthermore, differences in most CBCs were higher in men compared to women.
All analyses presented high heterogeneity in main and sensitivity analyses but no overall publication bias.
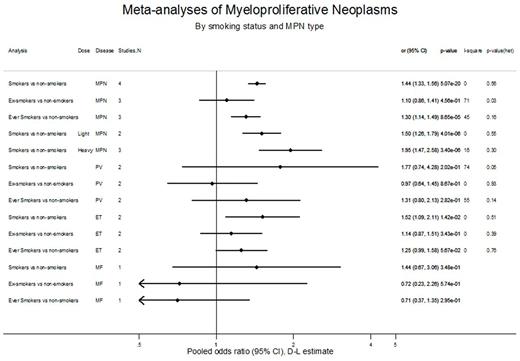
Myeloproliferative Neoplasms (MPN): We included 5 studies with a total of 1,368,738 individuals and 2017 MPN cases. 2 studies were prospective and 3 studies case-control. Pooled odds ratio for MPN were 1.44 (95%CI: 1.33-1.56; p-value=5*10(-20); I-square=0%, p(heterogeneity)=0.56) comparing smokers to non-smokers, 1.10(0.86-1.41; p-value=0.46; I-square=71%, p(heterogeneity)=0.03) comparing ex-smokers to non-smokers, and 1.30(1.14-1.49; p-value=8*10(-5); I-square=45%, p(heterogeneity)=0.16) comparing ever-smokers to never smokers.
Conclusion
Current smokers, ex-smokers, and ever-smokers have higher mean CBCs and an increased risk of MPN compared to non-smokers.
Hasselbalch: AOR Orphan: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.